Bariatric Surgery vs. GLP-1 Drugs: The Strongest Path to Lasting Weight Loss & Improvement in Related Health Conditions
September 12, 2025By: Janet Klein, MS, RDN, CDN, CDCES
Categories: Bariatric, Blog, Health & Wellness
 Janet Klein, MS RDN, CDN, CDCES, Bariatric Surgery and Obesity Medicine Program Director
Janet Klein, MS RDN, CDN, CDCES, Bariatric Surgery and Obesity Medicine Program Director
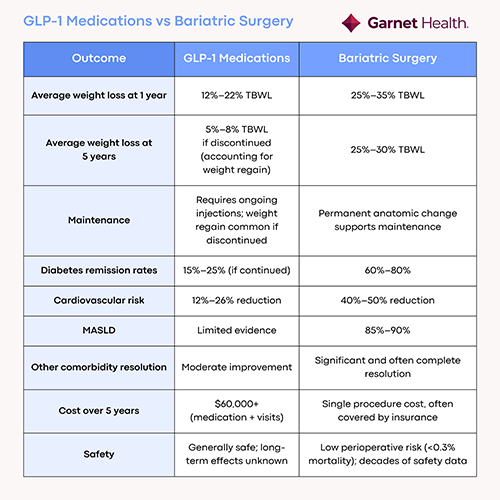
It may not be much of a surprise to hear that with the increased use of GLP-1s for weight loss, there has been a noted decline in patients undergoing bariatric surgery. But would it surprise you to learn that, in the long term, bariatric surgery provided better outcomes than GLP-1s for weight loss and weight-related health problems such as diabetes?
To be clear, this data targets obese individuals medically defined as having a BMI of 35 to 39.9, with weight-related health issues or a BMI equal to or greater than 40. However, according to the CDC, more than 40% of Americans are clinically obese (BMI over 30), which means truly knowing and understanding your options for optimal weight loss is vital in order to make the best decision to improve your health and well-being.
Obesity can be caused by unhealthy habits and is often genetic. Regardless of cause, if left unchecked, excess weight can contribute to chronic health conditions such as arthritis and other joint issues; cancer; chronic pain and reduced mobility; Type 2 diabetes; heart disease, such as coronary heart disease and hypertension; mental illness or eating disorders; sleep apnea and other sleep disorders; and stroke.
What are GLP-1s, and how do they work?
GLP-1s are prescription medications, such as Wegovy®, Ozempic® Mounjaro®, & Zepbound ® that mimic the action of the naturally occurring GLP-1 hormones in the body. They help with weight loss by reducing one’s appetite and increasing the feeling of being full, slowing digestion, and reducing what some refer to as “food noise.”
GLP-1s are a valuable, proven tool when part of a weight-management program that includes lifestyle changes such as healthier eating and increased activity. Average total body weight loss (TBWL) after one year on a GLP-1 semaglutide such as Wegovy® and Ozempic® is 12%–15%, and on a GLP-1 tirzepatide like Mounjaro®, & Zepbound ® is 21%.
But attempts to maintain that weight loss can mean ongoing, possibly lifelong, injections which can prove costly, and much of the weight lost can be regained in a relatively short period of time if the medication is stopped. Plateaus can be reached way before significant weight loss is achieved, especially with severely or morbidly obese patients who use these medications as first line treatment. There are also possible side effects such as nausea, vomiting, diarrhea and constipation.
What is bariatric surgery?
There are different types of bariatric surgery, but all are designed to physically alter aspects of your digestive system to make it easier for you to manage your weight.
Gastric Bypass: Reroutes food to a small stomach pouch so you take in fewer calories.
Gastric Banding: An adjustable band shrinks the stomach opening so you feel full sooner and eat less.
Gastric Sleeve: Removes most of the stomach, so you eat less and feel less hungry.
Bariatric surgery patients tend to see about five times more weight loss than weekly injections of GLP-1s at the end of two years according to a new study. Additionally, bariatric surgery is a one-and-done procedure, so maintenance, when coupled with lifestyle changes, is easier to accomplish, as the weight-reducing change is permanent.
When it comes to reduction of weight-related issues like diabetes, heart disease risks and metabolic dysfunction-associated steatotic liver disease (MASLD), formerly known as nonalcoholic fatty liver disease (NAFLD), bariatric surgery far outpaces GLP-1s in reduction, and often removal, of these risks.
There’s something for everyone.
If you have a BMI between 35 to 39.9, along with one or more health conditions, or a BMI of 40 or higher, consider consulting with a provider who can explain the advantages of both GLP-1 medications and bariatric surgery. Garnet Health is committed to providing all patients with a personalized plan to achieve their weight-loss goals including one of these options or in combination with each other to achieve maximum benefit.
Obesity medicine doctors at Garnet Health will create a plan unique to each patient’s goals and needs. While this may include prescribing GLP-1s for some patients, these medications are often a tool to help promote weight loss, but not a solution.
A good metric to consider is this: If an obese patient (BMI 30 to 34.9) is on a GLP-1 for six months and has not reached 10% TBWL, they should be referred back to their primary care provider to reassess their weight-loss plan. If a severely obese patient (BMI 35 to 39.9) with one or more health conditions, or a morbidly obese patient (BMI 40 or greater), has not reached 10% TBWL in six months, they should be referred for bariatric surgery.
Once a patient is referred, Garnet Health’s bariatric specialists will work with them at a pace that’s realistic and healthy, offering a variety of weight-management services, including:
- Bariatric seminars and preoperative bariatric education
- Bariatric surgery support groups
- Pre-surgical testing
- Bariatric surgery
Weight-loss surgery isn’t just about taking off weight, it can also be about taking back control of your life. If you want to learn more about the Bariatric and Obesity Medicine services at Garnet Health, visit garnethealth.org/bariatricprogram or call (845) 333-2123.
